Tips for Using your Electronic Health Record (EHR) for PCMH
An Electronic Health Record (EHR) is essential for a Patient-Centered Medical Home (PCMH) practice, both in obtaining recognition and more importantly in maintaining it. You can use your EHR to improve patient care, the efficiency of your practice, and the cost of care.
Help and Support
We are available to assist you with the PCMH process and quality improvement. This service is available to your practice at no cost.
To reach our team call 203.949.4194 or email pcmhglideapplication@chnct.org.
Getting Started with an EHR
Benefits of EHRs
There are multiple benefits to using an EHR, ranging from improving patient care through quality improvement to improving practice efficiencies and cost savings.
EHR BenefitsNational Adoption of EHRs
The Office of the National Coordinator for Health Information Technology is a resource to support the adoption of health information technology across the entire health system. It seeks to improve healthcare by promoting nationwide health information exchange in order to improve healthcare.
Health System Adoption of EHRsUsing Your EHR for Quality Improvement
Quality Improvement
Many EHRs can help you save time and money during the quality improvement process. EHRs can also make healthcare more convenient for providers and patients. Although each EHR system is unique, each system has tools to assist with quality improvement. Talk to your EHR vendor about the quality improvement tools that are available through your EHR.
Improved Care Using EHRsHealth IT Playbook
There is a growing nationwide focus on value and quality in the healthcare system, and clinicians now have access to incentives for practice transformation and care delivery. In this Playbook, you will find strategies, recommendations, and best practices to assist you in improving quality.
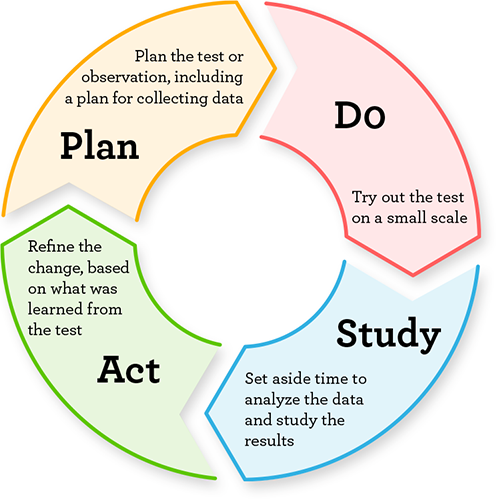
Health IT PlaybookPDSA: What it is and how it works
The Plan-Do-Study-Act (PDSA) cycle is a tool for continuous quality improvement. The goal of the PDSA cycle to test a change–by planning it, trying it, observing the results, and acting on what is learned.
PDSA CyclesPCMH and Your EHR
Choosing an EHR Vendor
There are several options for a practice interested in selecting a vendor. To help you learn about different EHRs and narrow your options before selecting an EHR vendor, you can use a vendor assessment. Click on the link below to learn more about the steps in choosing an EHR vendor.
Choosing a VendorNational Committee for Quality Assurance (NCQA) PCMH EHR Pre-validated Vendors
Many EHRs have the capability to provide reports and data required for NCQA PCMH recognition. Although it is not necessary to have a pre-validated EHR, NCQA provides a PCMH Vendor List to help practices meet PCMH program requirements with automatic credit. Find out if your EHR system is validated by NCQA for automatic credit toward PCMH criterion.
Pre-validated VendorsElectronic Clinical Quality Measures (eCQM)
The ability to share your clinical quality measures may provide your practice with additional revenue. Electronic Clinical Quality Measures (eCQMs) are standardized performance measures from EHRs or health information technology systems. In the future, practices will have the option to submit eCQMs to NCQA in support of their recognition process.
You will be able to submit identified measures through your EHR systems, health information exchanges, qualified clinical data registries, and data analytics companies as long as those vendors use the electronic specifications defined by the Centers for Medicare & Medicaid Services for the ambulatory quality reporting programs. More details about the data submission process to NCQA will be forthcoming.
https://ecqi.healthit.gov/ecqms
Source: ncqa.org
Benefits of Using eCQMs
- Access to detailed clinical data to assess treatment outcomes
- Reduce the burden of manual abstraction and reporting
- Access to real-time data for bedside quality improvement and clinical decision support
This portion of the HUSKY Health website is managed by Community Health Network of Connecticut, Inc.®, the State of Connecticut’s Medical Administrative Services Organization (ASO) for the HUSKY Health program. For the general HUSKY Health website gateway, please visit portal.ct.gov/husky. HUSKY Health includes Medicaid and the Children’s Health Insurance Program, and is administered by the Connecticut Department of Social Services (DSS).