Care Management
CHNCT’s Care Management program includes Intensive Care Management (ICM), and Transitional Care Management (TCM), which focus on the complex care management of members with multi-morbid conditions, barriers to optimal care, and psychosocial needs. ICM provides comprehensive case management services that aim to increase member engagement in ongoing care with a primary care provider (PCP), decrease potentially avoidable hospitalizations, and reduce health disparities through multi-disciplinary, person-centered care and care coordination. Transitional Care services support smooth transitions from a healthcare facility to home, and participation in recommended follow-up care. By responding to members’ individual needs, the Care Management program provides focused care coordination resulting in improved patient participation for better health.
Refer Members to ICM
If you have patients that would benefit from the additional support provided by ICM, call 1.800.440.5071 x2024, or fax a completed ICM Referral Form to 866.361.7242.
More Information
Elements of Care Coordination
The Care Management Team can help your patients by:
- Promoting the patient’s ability to engage with their care team and participate in recommended care
- Addressing barriers leading to gaps-in-care and promoting optimal use of benefits
- Providing individualized health coaching in the patient’s preferred language
- Supporting treatment plan progress and successful medication management
- Increasing patient self-management to reduce potentially avoidable hospitalizations
- Action planning to recognize warning signs of a worsening condition and seek early treatment
- Supporting successful care transitions by evaluating the patient’s understanding of discharge instructions, and ensuring recommended follow-up care is arranged
Community Health Worker Ambassador Program
Our certified Community Health Workers (CHWs) serve as ambassadors for the HUSKY Health program and help families access community resources for the services they need. They are committed to help building equity through diversity, inclusion, and community engagement efforts. They work to ensure that all members, regardless of ability, age, cultural background, ethnicity, faith, gender, gender identity, ideology, income, national origin, race, or sexual orientation have the opportunity to reach a better quality of health.
CHWs provide the following patient assessment and referral services:
- Childcare and parenting support
- Disability services and other related services
- Domestic violence support and legal services
- Educational and youth programs
- Employment services
- Housing, food, and clothing assistance
- And more
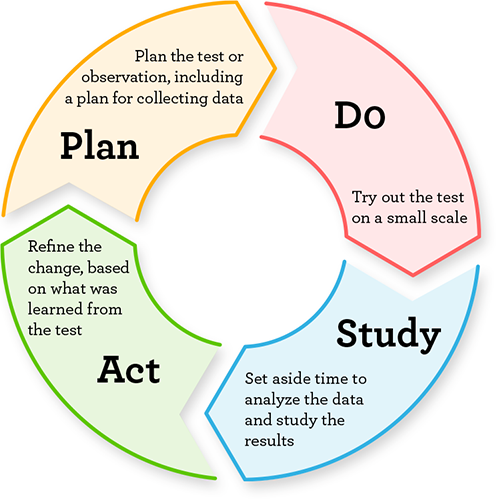
How Care Management Works
- Care Management nurses reach out to identified or referred members to offer participation in the Care Management program.
- A holistic assessment is conducted that evaluates a member’s medical, behavioral, and health-related social needs, self-care ability, screenings, and more.
- Care Management nurses work with providers, other agencies, and the multidisciplinary care team to help members access the care and programs they need to achieve their health goals.
- Care Management nurses support the provider’s plan of care for the member and provide education and tools to improve self-management.
- Members graduate from Care Management once they reach an optimal level of self-management and engagement in recommended care in partnership with their providers.
- If a hospital admission or emergency department visit should occur, Transitional Care nurses collaborate with members, caregivers, providers, and community agencies to ensure provider follow-up and services are in place.
This portion of the HUSKY Health website is managed by Community Health Network of Connecticut, Inc.®, the State of Connecticut’s Medical Administrative Services Organization (ASO) for the HUSKY Health program. For the general HUSKY Health website gateway, please visit portal.ct.gov/husky. HUSKY Health includes Medicaid and the Children’s Health Insurance Program, and is administered by the Connecticut Department of Social Services (DSS).